For many men, the word testosterone is shorthand for sex drive or muscle mass. However, testosterone shapes how multiple bodily systems function, and while present in women, it has a far greater influence on physical and physiological processes in men.
If you’re a man in your 30s, 40s, 50s, or beyond and you’re noticing persistent fatigue, loss of drive, weight gain, or changes in sexual health, understanding testosterone – and how it works, is an essential first step toward making informed decisions about your health.
This article explains what testosterone is, what it does, how levels change over time, and when it may be worth testing or seeking medical input.
What is testosterone?
Testosterone, often shortened to T, is a steroid hormone belonging to the androgen family. In men, it is produced primarily in the testes, with smaller amounts made by the adrenal glands. Its production is regulated by a tightly controlled hormonal feedback loop known as the hypothalamic–pituitary–gonadal (HPG) axis.
In simple terms:
- The hypothalamus signals the pituitary gland via release of gonadotropin-releasing hormone (GnRH)
- The pituitary releases luteinising hormone (LH) and follicle-stimulating hormone (FSH)
- LH and FSH act on the testes, LH stimulates the Leydig cells to produce testosterone whilst FSH stimulates the Sertoli cells to produce sperm.
This system keeps testosterone within a functional range. However, it becomes less efficient with age [1] and can be disrupted by illness, stress, obesity, or medications.
What does testosterone do in the male body?
Testosterone acts as a key regulator across multiple systems in the male body. From physical strength and metabolism to mood, energy, and cognitive health, its effects are wide-ranging and interconnected.
Physical health and body composition
Testosterone plays a major role in physical health, including:
- Muscle protein synthesis and strength maintenance
- Fat distribution, particularly abdominal fat
- Bone density
- Red blood cell production, influencing stamina and oxygen delivery
Low testosterone levels are associated with increased fat mass, weaker bones, and reduced muscle mass. These changes are often attributed to “normal ageing” but may reflect hormonal decline.
Sexual and reproductive health
Testosterone is essential for:
- Libido
- Erectile function
- Sperm production (in conjunction withFSH)
- Genital tissue health
While erectile dysfunction is not always caused by low testosterone, a deficiency makes sexual issues more likely.
Mood, motivation, and cognitive function
Testosterone has significant effects on the brain and research shows it influences:
- Motivation and goal-directed behaviour
- Confidence and emotional resilience
- Energy levels
- Cognitive processing speed and memory
Low testosterone has been linked with increased rates of depressive symptoms, apathy, and reduced sense of wellbeing [2].
Metabolic and cardiovascular effects
Low testosterone has been consistently linked with adverse metabolic changes and increased cardiovascular risk in men. Research shows that men with chronically low testosterone are more likely to develop:
- Insulin resistance
- Unfavourable cholesterol profiles
- Increased visceral fat
- Metabolic syndrome
All of these are established risk factors for type 2 diabetes and cardiovascular disease [3].
Importantly, this relationship is bidirectional. Conditions such as obesity and insulin resistance can suppress testosterone production, while low testosterone can further worsen metabolic health, creating a self-perpetuating cycle [4].
Read our guide to TRT and heart health for more information.
What is the difference between free and total testosterone?
When testosterone is measured in blood tests, results are usually reported as total testosterone, but this does not tell the whole story. Total testosterone is the amount of testosterone circulating in the bloodstream. Around 98% of testosterone is bound to either sex hormone-binding globulin (SHBG) or albumin, while only a small fraction remains unbound.
Free testosterone is not bound to any protein and, therefore, is biologically active – able to enter cells and exert its effects on muscles, bones, brain, and sexual tissues. Some testosterone loosely bound to albumin is also considered bioavailable, as it can readily dissociate and be used by the body. This distinction matters because conditions such as ageing, obesity, thyroid disease, and insulin resistance can increase SHBG levels, reducing free testosterone even when total testosterone appears normal [5].
Testosterone levels in men – what changes with age?
Testosterone levels in men are not static; they follow a predictable life-course pattern. In the late teens to early 20s, levels typically peak, before beginning a gradual decline.
From around the age of 30, total testosterone falls by an average of 1% per year, while free testosterone often declines more steeply due to rising levels of SHBG. This means that even when total testosterone is “within range,” the amount available to the body may be much lower.
Significantly, age-related decline does not affect all men equally. Genetics, body composition, sleep, stress, alcohol intake, and overall health all influence how quickly testosterone levels fall. As a result, two men of the same age with similar testosterone results may experience very different symptoms.
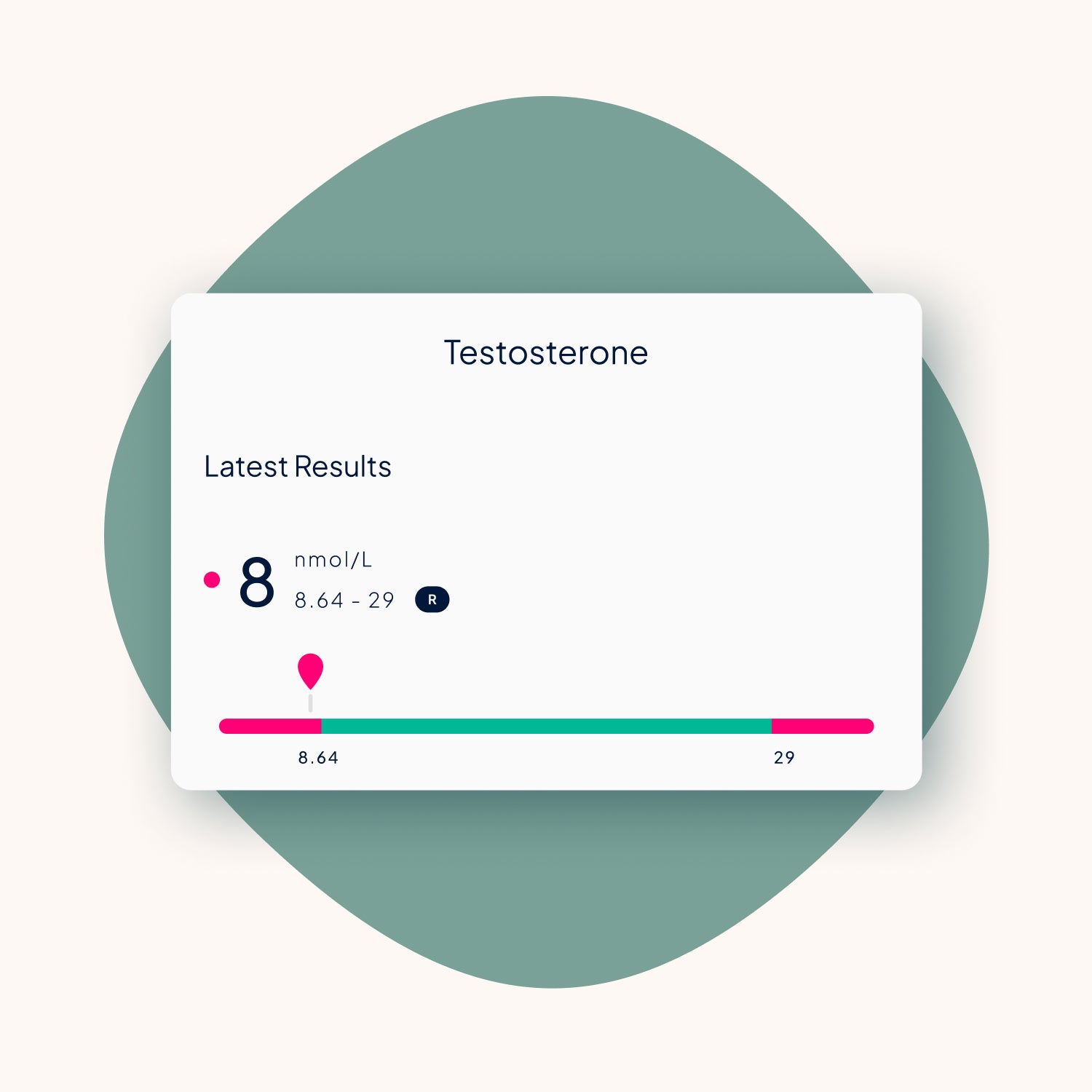
Testosterone is measured in nanomoles per litre (nmol/L).
|
Age in years |
Men (nmol/L) [1] |
|
2 – 10 |
<0.24 – 0.35 |
|
11 – 15 |
<0.24 – 26.25 |
|
16 – 17 |
7.92 – 27.0 |
|
18 – 49 |
8.7 – 29.0 |
|
50+ |
6.7 – 25.7 |
Symptoms matter as much as numbers
Laboratory reference ranges are broad. Two men with the same testosterone level may feel very different. This is why clinical guidelines emphasise that symptoms and testosterone results – not numbers alone, should guide decisions [5].
Signs and causes of low testosterone
Low testosterone can develop gradually, with symptoms that are often subtle or easily attributed to stress or ageing. Understanding the common signs and underlying causes can help identify when further testing or medical advice may be appropriate.
Common symptoms of low testosterone
Men with low testosterone may experience:
- Persistent fatigue or low energy
- Reduced motivation or drive
- Low libido
- Erectile difficulties
- Loss of muscle mass
- Increased body fat
- Low mood or irritability
- Poor concentration
You can learn more from our dedicated guide on signs and symptoms of low testosterone.
Why testosterone levels can drop
Low testosterone can result from:
- Age-related decline
- Obesity and insulin resistance
- Chronic stress and poor sleep
- Excess alcohol consumption
- Certain medications (e.g. opioids, steroids)
- Testicular or pituitary disorders
Often, multiple factors interact rather than a single cause being responsible.
When should men consider testosterone testing?
Men may consider testosterone testing when they experience persistent signs of low testosterone that affect daily life. Clinical guidelines recommend that testosterone testing should be prompted by symptoms rather than age alone, as testosterone levels and symptom burden do not always align [5].
Testing is recommended for men with certain risk factors, such as obesity, type 2 diabetes, metabolic syndrome, long-term opioid use, or a history of testicular or pituitary disorders.
For the most reliable results, testosterone is usually measured in the morning, ideally before 11 am, when levels are naturally at their highest. If an initial result comes back low, a follow-up test is required to look at other possible causes for your symptoms, as well as confirming your testosterone is low. These tests should be 4 weeks apart as testosterone levels can vary greatly on a daily basis.
For more information, see our guide to taking a testosterone blood test.
Optimising testosterone naturally vs. medical treatment
When testosterone levels are lower than expected, there are several options available depending on symptoms, results, and overall health. Understanding the difference between natural remedies and medical treatment helps men make informed, appropriate choices about next steps.
Lifestyle adjustments
Before considering medical treatment, clinicians often assess several factors, including:
- Body composition and weight management
- Sleep quality
- Resistance training and physical activity
- Drug and alcohol intake
- Stress levels
Lifestyle improvements can raise testosterone levels in some men, particularly where obesity or sleep deprivation is a factor.
Testosterone supplements
Over-the-counter testosterone supplements are widely marketed to improve levels, but evidence for their effectiveness is limited. Most supplements do not meaningfully increase testosterone in men with normal hormone function, and any minor effects observed are usually linked to correcting an underlying deficiency – such as vitamin D or zinc, rather than directly raising testosterone levels [5].
This is why blood testing is essential. It helps determine whether symptoms are linked to testosterone deficiency or another cause and avoids unnecessary or ineffective supplementation.
For more information, read our guide to testosterone supplements.
Testosterone replacement therapy (TRT)
When symptoms persist and blood tests confirm deficiency, testosterone replacement therapy (TRT) may be considered. TRT aims to restore testosterone to physiological levels, not to exceed them.
Treatment options include:
- Injections
- Gels
- Tablets
- Creams
TRT requires medical supervision and regular monitoring. You can learn more in our articles on what is testosterone replacement therapy (TRT)? and how to get TRT in the UK.
TRT vs anabolic steroids
TRT and anabolic steroids are essentially the same thing, although the term anabolic steroids can cover compounds that are based on testosterone but not available for prescription. The main difference comes down to dose; testosterone is an anabolic steroid, but dosages tend to be much higher when used for performance enhancement vs what is required to replace a normal level of testosterone.
|
TRT |
Anabolic steroids |
|
Prescribed for testosterone deficiency |
Used for performance enhancement |
|
Physiological dosing |
Doses that raise T levels above the body’s natural range |
|
Medically monitored |
Often unsupervised |
|
Health-focused |
Performance-focused |
Confusing the two leads to unnecessary fear and misinformation. For a detailed comparison, see our guide to TRT vs steroids.
Fertility and long-term considerations of TRT
While TRT can effectively relieve symptoms of a deficiency, testosterone that’s introduced to the body from an external source can suppress the natural production of LH and FSH. This can significantly reduce or halt sperm production, sometimes leading to temporary infertility [6].
When appropriately prescribed and supervised, TRT can be used long term, but it should always be seen as a medical therapy rather than a lifestyle supplement, with risks and benefits reviewed.
For more information, read our guide to fertility and TRT.
Testosterone shapes how the body feels and functions, and by understanding its role and when to seek advice, men can move away from guesswork and support their long-term wellbeing.
References:
-
Smith, J. (2024) What is a normal testosterone level for your age? Medichecks. (Accessed: 6 January 2026)
-
Handelsman, D.J. and Wittert, G.A. (2024) ‘Testosterone and depression symptoms in aging men’, The Journal of Clinical Endocrinology & Metabolism. (Accessed: 6 January 2026)
-
Corona, G., Monami, M., Rastrelli, G., Abersa, A., Tishova, Y., Saad, F., Lenzi, A., Forti, G. and Maggi, M. (2011) ‘Testosterone and metabolic syndrome: a meta-analysis study’, Endocrine Abstracts, 26, p. P315. (Accessed: 8 January 2026).
-
Kelly, D., Jones, T. (2015) ‘Testosterone and Obesity’, Obesity Reviews, (Accessed: 9 January 2026).
-
Bhasin, S., Brito, J.P., Cunningham, G.R., Hayes, F.J., Hodis, H.N., Matsumoto, A.M., Snyder, P.J., Swerdloff, R.S. and Wu, F.C.W. (2018) ‘Testosterone therapy in men with hypogonadism: An Endocrine Society clinical practice guideline’, Journal of Clinical Endocrinology & Metabolism. (Accessed: 7 January 2026).
-
Trost, L.W. and Mulhall, J.P. (2016) ‘Challenges in testosterone therapy: fertility and cardiovascular risk’, Nature Reviews Urology, 13(6), pp. 309–322. (Accessed: 9 January 2026).




Share:
How do you know if your testosterone is low?
Is male menopause (andropause) real?