Many men in their 40s, 50s, and 60s describe feeling unlike themselves – energy dips, motivation wanes, sleep becomes fragmented, and mood shifts feel unfamiliar. Libido may also change, sometimes subtly, sometimes abruptly.
So, are these all signs of the so-called male menopause (aka manopause), and does it play out in the same way as the female menopause?
Is the male menopause real?
Men don't experience menopause in the same way as women, but they do undergo age-related hormonal changes that can affect physical and psychological health.
You may not notice shifts in your mood and energy suddenly or simply put any changes down to getting older. But, whether you or your partner notice changes to your mood, energy, or libido, a natural decline in testosterone may be able to explain them.
Understanding this decline in testosterone, and the difference between the menopause and manopause, matters and helps make sense of symptoms without unnecessary fear. It also avoids misleading comparisons and supports informed conversations with healthcare professionals.
Low testosterone (andropause) vs male menopause: medical reality and popular perception
The terms andropause and male menopause are often used interchangeably, but one is a medical term and the other is a label people use. Understanding the distinction helps avoid confusion, unnecessary anxiety, and misinterpretation of midlife health changes in men.
Andropause: the medical understanding
Andropause is also known as late-onset hypogonadism (low testosterone with problematic symptoms), or androgen deficiency in ageing men (ADAM).
Low testosterone is a recognised clinical condition in which men experience testosterone levels below the normal range alongside specific physical, sexual, or psychological symptoms.
Some people have coined the male menopause phrase as testosterone production in men naturally declines with age, typically beginning around age 30-40 [1], which is a similar timeframe for when some women enter perimenopause.
Importantly, low testosterone is not something that is inevitable with ageing [2]. It’s diagnosed only when testosterone levels are repeatedly confirmed as being low, and they are accompanied by testosterone-related symptoms.
Management focuses on identifying underlying contributors such as obesity, chronic illness, medication effects, or sleep disorders before considering hormone-based treatment.
Our guide to testosterone and why it matters for men provides more information on this vital hormone.
Male menopause: the popular interpretation
Male menopause is a non-clinical term that has developed in popular culture to describe midlife changes in men. It’s often portrayed as the male counterpart to female menopause. In reality, this comparison is biologically inaccurate.
Female menopause involves a relatively rapid and permanent cessation of ovarian function. This leads to a sharp decline in oestrogen and progesterone and the end of fertility. Male reproductive hormone production, by comparison, continues throughout life, and testosterone decline is gradual, variable, and frequently asymptomatic [1].
The popular idea of male menopause tends to overgeneralise symptoms, attributing common midlife experiences – such as stress, fatigue, relationship changes, or psychological adjustment, to hormonal failure. This can obscure other significant health issues and oversimplify complex emotional and social factors that often coincide with midlife.
Why the distinction matters
Merging andropause with male menopause can result in misunderstandings and inappropriate self-diagnosis. Recognising it as a medically defined condition helps ensure men experiencing andropause receive appropriate assessment, evidence-based care, and realistic expectations about ageing and health.
In short: andropause is a medically defined condition affecting a minority of men; male menopause is a cultural label that oversimplifies midlife changes.
Male menopause vs female menopause
Understanding how male hormonal ageing differs from female menopause helps clarify why the terms are not interchangeable.
Female menopause
- Ovarian function stops
- Sharp hormonal change
- Fertility ends
- Universal life stage
Andropause
- Testosterone declines gradually
- Slow, variable change
- Fertility usually continues
- Not inevitable
While both involve hormones and ageing, the underlying biology and psychological impact are fundamentally different.
Do men go through menopause emotionally?
It is common for partners to sense changes in emotional closeness, confidence, or resilience as men move through midlife. These emotional changes are real and meaningful, but they aren’t always caused by hormones alone.
This stage of life can also coincide with several factors that cause a shift in emotions, including:
- Career pressure or plateauing
- Caring responsibilities
- Relationship transitions
- Health concerns
- Awareness of ageing and mortality
Common signs of andropause
Andropause is characterised by a combination of persistently low testosterone levels and associated symptoms of low testosterone.
It’s important to know that low testosterone symptoms can be non-specific and mirror common changes in the midlife. Symptoms alone aren’t enough to diagnose andropause, which is why testing testosterone levels is essential.
Not all men with age-related testosterone decline will experience symptoms, and symptoms alone are not sufficient for diagnosis.
Sexual symptoms
Sexual changes are among the most consistently reported features of clinically significant testosterone deficiency. These may include:
- Reduced libido
- Erectile dysfunction or reduced sexual satisfaction
Population-based studies have shown that sexual symptoms, particularly low libido and erectile difficulties, are the symptoms most strongly associated with low testosterone levels in ageing men [2].
Physical symptoms
As testosterone levels decline, some men may experience:
- Reduced muscle mass
- Increased body fat
- Decreased bone mineral density
These physical changes tend to develop gradually and may be influenced by lifestyle factors such as physical activity, nutrition, and overall health status.
Psychological symptoms
Testosterone also affects brain function and mood regulation. Psychological and cognitive symptoms associated with andropause may include:
- Low mood or depressive symptoms
- Irritability or reduced tolerance
- Difficulty concentrating
- Reduced motivation or confidence
Symptom relevance
However, the same symptoms could be indicative of other issues, such as:
- Depression or anxiety
- Thyroid disorders
- Sleep apnoea
- Vitamin deficiencies
- Cardiovascular disease
- Chronic stress or burnout
Research indicates that only a minority of men develop a symptom pattern that meets strict diagnostic criteria for andropause. Symptoms are most clinically relevant when they are persistent, impactful, and occur alongside confirmed low testosterone levels.
Age-related testosterone decline patterns
Across a man’s lifetime, testosterone follows a recognised pattern – rising through puberty, peaking in early adulthood, and slowly decreasing with age. This gradual fall is entirely natural. However, the speed of the testosterone decline and how much it impacts varies widely between individuals.
Studies show that, generally, testosterone levels decrease by approximately 1–2% per year from around the age of 30–40. However, for most men, this decline is mild and symptom-free. Free and bioavailable testosterone decline more steeply due to age-related increases in sex hormone-binding globulin (SHBG) [1].
Importantly, testosterone decline is not solely driven by chronological age, and can be impacted by several factors, including:
- Obesity
- Type 2 diabetes
- Chronic inflammatory conditions
- Long-term stress
- Poor sleep quality
- Certain medications.
In contrast, men who maintain good cardiometabolic health often preserve testosterone levels well into later life [2].
Age-related testosterone decline is best understood as a gradual, multifactorial process influenced by biological ageing, health status, and lifestyle factors. Recognising these patterns helps distinguish normal ageing from pathological hormone deficiency and supports more accurate clinical assessment.
How andropause is diagnosed
There is no single test for andropause.
Diagnosis involves:
- A detailed clinical history
- Assessment of symptoms and their impact
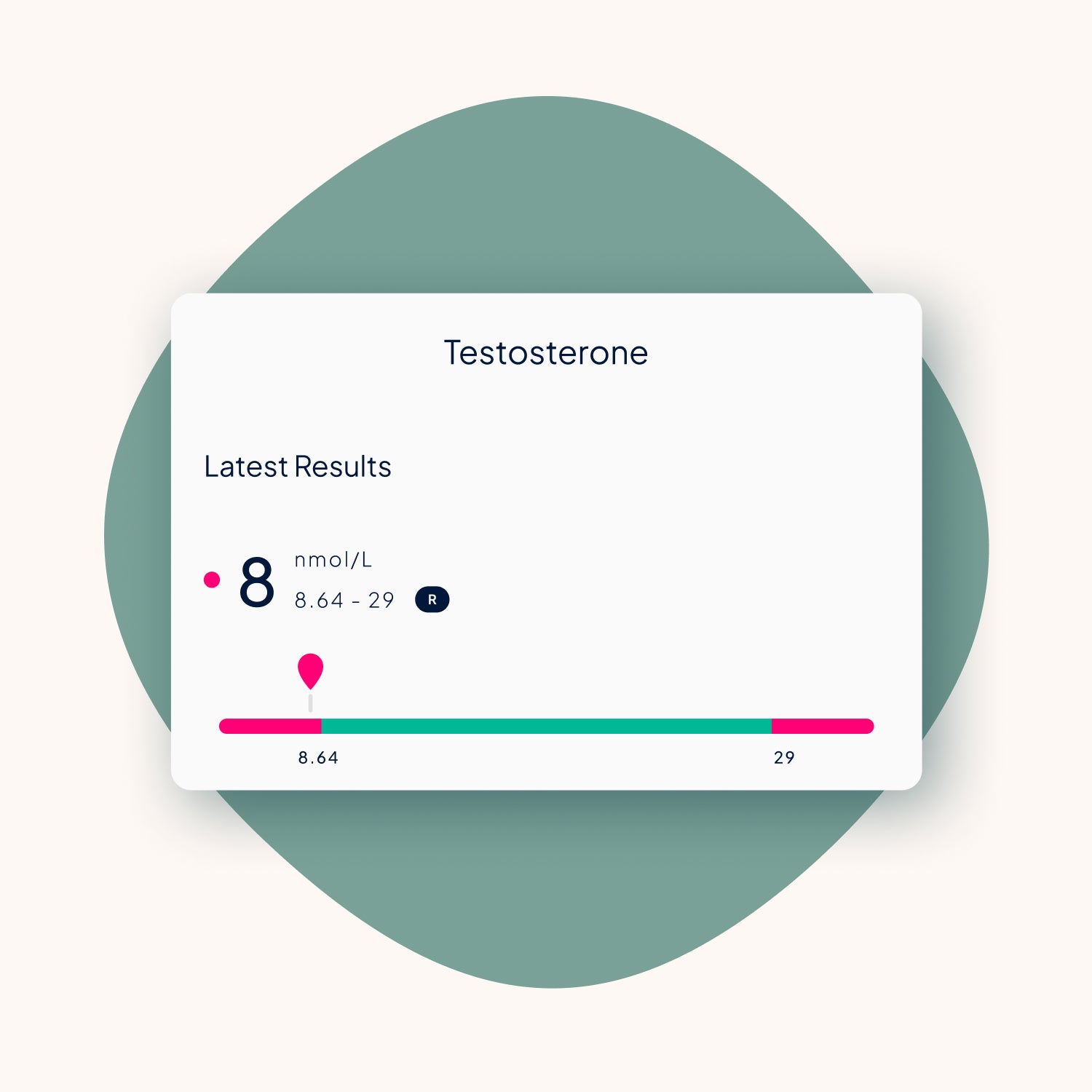
- Blood tests showing consistently low testosterone
- Exclusion of reversible or alternative causes
Blood tests are usually taken in the morning, when testosterone levels are highest, and are then repeated to confirm the results. A diagnosis is based on both numbers and symptoms.
When to seek medical advice
It may be worth seeking clarity from a healthcare professional if:
- Symptoms persist for several months
- Quality of life or relationships are affected
- Sexual function changes significantly
- Mood symptoms are pronounced or worsening
Where TRT fits in
TRT, or testosterone replacement therapy, can treat andropause. The aim of treatment is to bring testosterone levels back into a healthy range and it may be prescribed for men with:
- Confirmed low testosterone
- Persistent, clinically significant symptoms
- No contraindications
Our guides provide more information about what TRT is, its benefits, and its risks.
Talking about male menopause with your partner
Partners are often the first to notice changes, sometimes well before people recognise or acknowledge themselves. Having open, honest conversations about these shifts can prevent misunderstandings, reduce misplaced blame, and create space for a more supportive relationship and shared decisions about health.
Helpful approaches include:
- Framing changes as shared challenges, not personal failings
- Avoiding assumptions about hormones being the sole cause
- Encouraging medical evaluation rather than self-diagnosis
- Recognising the emotional impact of midlife transitions
Testosterone decline with age is real, but it does not follow the same pattern as female menopause, nor does it affect all men in the same way. Making this distinction helps ensure that midlife health concerns are properly explored and managed using evidence-based approaches, rather than reduced to a single, catch-all explanation.
If symptoms are affecting your quality of life, a simple blood test can help clarify whether testosterone levels are contributing.
References
- Harman, S.M., Metter, E.J., Tobin, J.D., Pearson, J. and Blackman, M.R. (2001) ‘Longitudinal effects of aging on serum total and free testosterone levels in healthy men’, Journal of Clinical Endocrinology & Metabolism. (Accessed 19 January 2026)
- Wu, F.C.W., Tajar, A., Beynon, J.M., Pye, S.R., Silman, A.J., Finn, J.D., O’Neill, T.W., Bartfai, G., Casanueva, F.F., Forti, G., Giwercman, A., Han, T.S., Kula, K., Lean, M.E.J., Pendleton, N., Punab, M., Boonen, S., Vanderschueren, D., Labrie, F. and Huhtaniemi, I.T. (2010) ‘Identification of late-onset hypogonadism in middle-aged and elderly men’, New England Journal of Medicine. (Accessed 19 January 2026)




Share:
What is testosterone and why it matters for men’s health