Testosterone replacement therapy (TRT) is an increasingly popular treatment for low testosterone (low T) in men. It can lead to significant improvements in symptoms like erectile dysfunction, low libido, depressed mood, and low energy.
As with most treatments, it’s subject to its fair share of misinformation and misconceptions. If you’ve been diagnosed with low T, or have symptoms, and you’re considering TRT, we’ll help you sort the facts from the fiction.
- Myth 1: TRT causes heart attacks
- Myth 2: TRT causes prostate cancer
- Myth 3: TRT is the same as taking anabolic steroids
- Myth 4: TRT is only for men with erectile dysfunction
- Myth 5: TRT causes infertility
- Myth 6: All forms of TRT are the same
- Myth 7: TRT is just for older men
- How to test your testosterone levels
7 myths about testosterone replacement therapy (TRT)
Myth 1: TRT causes heart attacks - what the research says
The most comprehensive research review to date found no link between TRT and an increased cardiovascular disease risk [1]. In fact, there’s evidence that restoring testosterone to healthy levels with TRT may even reduce your chance of heart attacks and stroke [2].
Perhaps this is not surprising when you consider the long-established link between low testosterone and heart disease [3].
This misconception is based on a handful of studies, conducted around 10 years ago, which linked TRT with an increased risk of cardiovascular disease. However, this research was heavily criticised for numerous flaws — not least that around 100 men in one of the studies were later reported to be women [4].
TRT may increase your haematocrit level, which can thicken the blood and make it more prone to clotting [5]. So, it’s important that haematocrit is monitored while taking TRT, and it should remain below 54%, according to BSSM guidelines [6].
Takeaway: For most men, TRT poses no increased risk of cardiovascular events, and in some cases, it may improve heart health. As with any new treatment, a doctor will help you weigh up the risks and benefits, based on your individual circumstances.
Myth 2: TRT and prostate cancer risk
The idea that TRT can cause or accelerate prostate cancer arose from a study exploring the effect of chemical castration on the progress of this disease in men [7]. The study found that halting the production of sex hormones (including testosterone) could slow disease progression.
Based on these findings, scientists reasoned that giving men testosterone could cause the opposite to happen — that it could cause or accelerate prostate cancers.
However, recent evidence indicates that TRT is unlikely to increase your risk of developing prostate cancer or cause low-grade cancers to spread [8].
Caution is advised for men who already have the condition. Current British Society for Sexual Medicine (BSSM) guidelines recommend that TRT should not be prescribed for men with more aggressive forms of prostate cancer, likely to spread outside the prostate [6].
Find out more about TRT and prostate health.
Takeaway: There's no compelling evidence that TRT increases the risk of prostate cancer. However, TRT can increase prostate-specific antigen (PSA) levels, so TRT prescribers must consider whether an increase is normal or warrants further investigation. In the latter scenario, sometimes prostate cancer is found. Hence, TRT may 'unmask' a prostate cancer that was there before starting treatment.
Myth 3: TRT vs anabolic steroids - key differences
TRT and anabolic steroids are both forms of exogenous testosterone (testosterone made outside the body), however, there’s a big difference between them.
The two main differences between TRT and anabolic steroids are that TRT is medically prescribed. In contrast, steroids are taken without formal medical guidance, and involve a much higher dose of testosterone than TRT.
The two main differences between TRT and steroids:
- Usage: TRT is a medically prescribed treatment, carefully monitored by doctors. Its purpose is to restore testosterone to healthy levels and improve symptoms of testosterone deficiency (TD). Steroids are typically taken by athletes and bodybuilders to excessively boost their testosterone levels to help build muscle and improve athletic performance.
- Dosage: taking anabolic steroids typically involves much higher doses of testosterone than TRT, sometimes around 100 times higher. This can cause potentially serious side effects and health complications, such as infertility and heart problems [9].
Takeaway: There’s a world of difference between taking TRT and taking steroids. If you’re taking TRT for TD, your testosterone levels should be regularly monitored to check you’re taking the right dosage. This ensures optimum safety and minimises your risk of side effects.

Myth 4: TRT is only for men with erectile dysfunction
One of the primary concerns of men taking TRT is indeed erectile dysfunction (ED), which can be an extremely distressing problem. However, there are many other symptoms of low testosterone that TRT can help to improve.
It could help you regain your energy levels, and restore your sex drive, and you may even notice a drop in body fat and the development of lean muscle because of taking TRT.
Takeaway: If you’re experiencing any symptoms of low testosterone, don’t ignore them. If your testosterone levels are too low for your age, treatment can help to improve your health and quality of life.
Myth 5: TRT and fertility concerns
One of the problems with TRT is that it markedly reduces fertility. That’s why your TRT prescriber will discuss family planning with you before starting treatment. If you’re looking to have children in the very near future, they may advise that you postpone treatment.
If you’re taking TRT and thinking of having children in the years ahead, most experts agree on protecting your fertility by taking human chorionic gonadotropin (HCG). HCG is a type of hormone, typically injected subcutaneously, three times a week. It can help reduce shrinkage of the testicles and stimulate sperm production, preserving fertility.
While HCG is effective for most men, it can’t guarantee that you’ll have children. Fertility is complex and dependent on many factors including your baseline sperm health as well as your partner’s reproductive health.
Even after stopping TRT, fertility can take six months to a year to return. And in some cases, fertility problems persist. Therefore, it’s important you discuss this with your prescriber before starting treatment.
Learn more about protecting fertility on TRT.
Takeaway: While taking TRT, you can monitor hormones that impact fertility with regular blood testing. If fertility is a concern for you, discuss this with your TRT prescriber before starting treatment. If you’re planning to have a baby in the near future, there are alternative treatments and strategies to manage low testosterone that might be more suitable.
Myth 6: Different types of TRT
TRT is available in many different forms including:
- Injections
- Pills
- Topicals, such as skin patches and gels
There are pros and cons for each TRT form. For example, injections might produce more reliable testosterone concentrations, but for some men, pills might be a better choice for their convenience.
The most common forms are injections and gels, but there’s no consensus on which is most effective. The key is to find what works best for you.
Find out more about the different types of TRT.
Takeaway: There’s no one-size-fits-all solution when it comes to TRT. Your doctor will work with you to select the best treatment for your unique needs, based on your preferences, goals, and response to the treatment.
Myth 7: TRT is just for older men
Testosterone levels naturally decline with age, but that doesn’t mean TRT is only for older men. In fact, low testosterone can affect men of all ages — and low T can lead to significant symptoms like fatigue, depression, reduced libido, and impaired physical performance, which can impact your overall quality of life.
If you’re in your 20s or 30s and suspect you may have low testosterone, it’s worth getting tested. You may benefit from TRT, and treatment could help improve your symptoms.
Find out what's an ideal testosterone level on TRT.
Takeaway: Low testosterone can affect men of any age. If you’re experiencing symptoms of low T, talk to a doctor to see if TRT could be a helpful treatment.
How to test testosterone levels from home
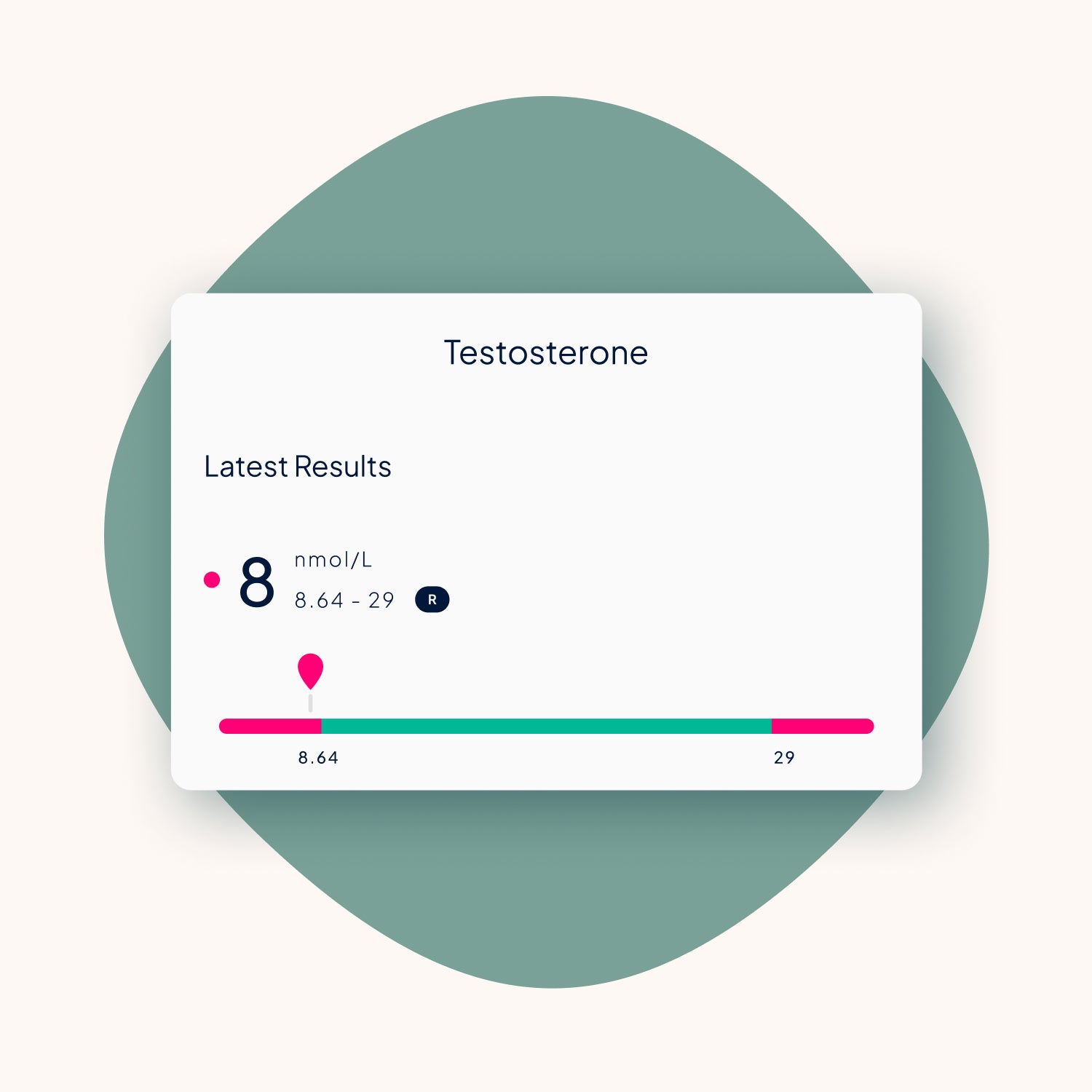
The only way to confirm whether your testosterone levels are low is with a Testosterone Blood Test. A doctor can help guide you on the next steps and make sure any symptoms you’re experiencing are due to low testosterone, not another underlying health issue.
Once you’ve confirmed you have low T, your doctor will discuss your treatment options with you, including the various forms of TRT available. Testing should be done regularly to ensure you’re maintaining safe, healthy testosterone levels.
The bottom line on TRT
Low testosterone is a serious condition, and TRT can be an effective treatment for improving quality of life. However, there are plenty of misconceptions surrounding the treatment.
By understanding the facts, you can make an informed decision about whether TRT is right for you. Always consult a doctor who is knowledgeable in testosterone therapy, and take the time to discuss your symptoms and options.
At Leger, we specialise in testosterone replacement therapy and our expert team is here to guide you every step of the way.
References
- Mohamad, M. et al., “Cardiovascular outcomes and testosterone replacement therapy in men: A systematic review and meta-analysis.” JAMA, 2016.
- Vigen, R. et al., “Testosterone therapy and cardiovascular events among men with low testosterone levels.” JAMA, 2013.
- Zhaoyang, L. et al., “Low testosterone levels and cardiovascular disease risk: A meta-analysis.” Journal of Clinical Endocrinology & Metabolism, 2016.
- Clark, J. et al., “Errors in research: The case of a study on testosterone therapy.” J Clin Endocrinol Metab, 2018.
- Rossi, G. et al., “Impact of testosterone replacement therapy on haematocrit levels: A review of the literature.” Andrology, 2020.
- BSSM (British Society for Sexual Medicine) guidelines on testosterone therapy, 2021.
- Geller, J. et al., “The effect of testosterone therapy on prostate cancer,” J Urology, 2009.
- Bhattacharya, D. et al., “Testosterone replacement therapy and prostate cancer: Evidence from recent research,” Urology, 2017.
- Pope, H. et al., “Anabolic steroids and cardiovascular disease,” British Journal of Sports Medicine, 2019.





Share:
TRT and type 2 diabetes: understanding the link
TRT and heart health: what’s the link?